Previous Page
${prev-page}
Next Page
${next-page}


Background and Overview of the Value-Based Arrangements Guide
Background and Overview of the Value-Based Arrangements Guide
D. What Is Value-Based Care?
Value-based care is the intended catalyst for health care in the United States to transition from volume to value. On the surface, the concept seems rather simple. Rather than reward health care providers simply for seeing patients and performing procedures and diagnostics, health care providers should be rewarded for providing better care for individuals and populations at a lower cost. These were the five original value-based programs initiated by the Centers for Medicare & Medicaid Services and payers:
• End-Stage Renal Disease Quality Incentive Program;
• Hospital Value-Based Purchasing Program;
• Hospital Readmissions Reduction Program;
• Value Modifier Program (also called the Physician Value-Based Modifier);
• Hospital-Acquired Condition Reduction Program.
E. Key Considerations
Historically, value-based care and value-related concepts have neither significantly moved the needle in negotiating reimbursement arrangements with health insurance payers nor resulted in significant shifts in care delivery. The emphasis on unit production has not provided systems with sufficient latitude to reward physicians for adopting different approaches for managing the health of a population — though this is shifting with the introduction of care coordination CPT® codes in the past few years. By contrast, utilization-focused metrics have been the primary concern within value-based contracts (i.e., screenings, immunizations and wellness visits). Many health systems believe that their portfolios contain insufficient revenue tied to value-based populations and are willing to consider innovative reimbursement arrangements, provided there is clear quality improvement and a promise of economic return.
Several dynamics exist in today’s health care market that suggest value-based care models will continue to be key levers in transforming health care from volume to value. Among the most recent drivers, the economic uncertainty of fee-for-service contract arrangements during the COVID‑19 pandemic has resulted in significant financial pressures among hospitals, health systems and academic medical centers, as high-revenue-generating services such as elective surgeries have been deprioritized in favor of lower-revenue-generating services such as caring for patients with COVID‑19. See figure 1 for additional details about current market forces indicating a continued transition toward value-based care models.
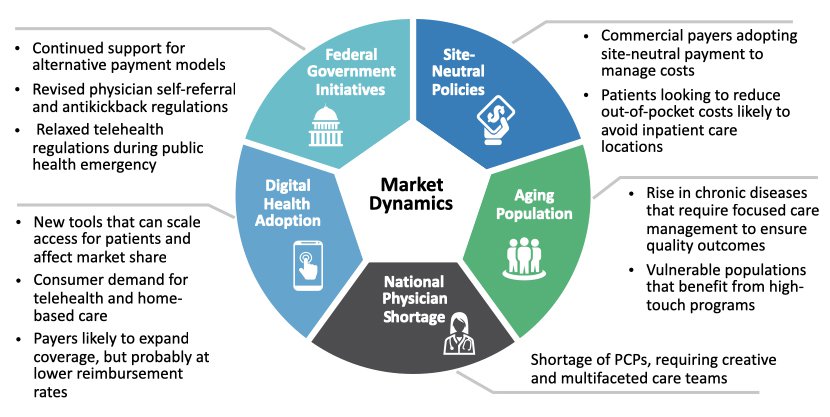
FIGURE 1: Value-Based Care Market Dynamics