Previous Page
${prev-page}
Next Page
${next-page}


Please Tell Us What You Think

Thank you for your interest in the Value-Based Arrangements Guide. Please complete this short survey to let us know what you think. Your feedback is instrumental in helping to shape future versions of this and other educational resources being developed as part of IDSA’s Physician Compensation Initiative.
The survey should take only 5 minutes to complete.
Open Survey
Background and Overview of the Value-Based Arrangements Guide
Background and Overview of the Value-Based Arrangements Guide
F. Metrics and Compensation
ID physicians impact the quality of health care both at the patient and health care system level. However, there is a lack of relevant measures available to largely hospital-based cognitive specialists including ID physicians. Aside from HIV and hepatitis C virus quality measures, which are meaningful to only a small proportion of ID physicians in the outpatient setting who focus on these disease areas (as opposed to general ID), there are very few ID-specific measures on which ID physicians can report to avoid payment penalties. ID physicians are not “proceduralists,” but rather nonproceduralists/cognitive physicians who provide most of their services using Evaluation & Management codes. Across all ID physicians in clinical practice, many E/M codes billed are for services provided in the inpatient setting (e.g., 82% of 2020 Medicare claims billed by ID physicians were at the facility place of service). The unique billing and practice patterns of ID physicians have made it challenging to develop additional quality measures that are feasible to report under value-based payment programs.
For more than a decade, IDSA has dedicated efforts to develop ID-relevant clinical quality measures, such as the 72-Hour Review of Antibiotic Therapy for Sepsis, Appropriate Use of Anti-MRSA Antibiotics and Appropriate Treatment of Initial Clostridium difficile Infection, to help fill this gap but has consistently been rejected by CMS when the measures were submitted for the Annual Call for Measures.
Nonetheless, there is an opportunity to develop new measures with clear attribution to ID activities, if the metrics are aligned with the six domains of health care quality (AHRQ and IOM/NAS), as defined below:
• Safe: avoiding harm to patients from the care that is intended to help them;
• Effective: providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and misuse, respectively);
• Patient centered: providing care that is respectful of and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions;
• Timely: reducing waits and sometimes harmful delays for both those who receive and those who give care;
• Efficient: avoiding waste, including waste of equipment, supplies, ideas and energy;
• Equitable: providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location and socioeconomic status.
G. Group and Individual Considerations
ID physicians have a unique opportunity to be incentivized through a mixture of group and individual performance. These types of goals incorporate the inclusion of a mixture of rewarding for individual performance and rewarding for group performance. The group goals can span multiple specialties and patient modalities, truly incentivizing team-based behaviors. A combination of individual and group metrics should be incorporated in a robust value-based arrangement design.
From a group perspective, it is important to recognize team-based care approaches and subspecialization. Further, group goals mitigate internal competition and may be applied to both volume- and value-based incentives.
Individual metrics, alternatively, need to be aligned with individual effort, and typically a combination of quality and throughput types of performance. These metrics are most successful when the intention is to recognize individual contributions and emphasize personal control, mitigating the “free rider” effect.
For ID, there are two basic approaches for establishing a pathway toward participation in value-based reimbursement programs and concepts.
1. Development of ID-Specific Measures
To date, there are no broadly applicable value-based programs designed specifically to capture the value of ID physician activities. However, developing metrics may be possible for rare diseases or for care that is only managed by ID physicians. Outpatient parenteral antibiotic therapy, for example, is an area in which outcome measures have not been fully developed and would be easily attributable to ID physician activities. HIV, like OPAT, is ID specific and actually does have broadly accepted quality measures. Additionally, medication allergies, especially documentation and verification of antimicrobial allergies, can have a major impact on antimicrobial selection and institutional costs and can be ID specific.
2. Institutional or Group Measures
In contrast to ID-specific measures, there are several quality metrics and outcomes measures for which ID physician involvement tends to improve outcomes. Examples include CAUTI, CABSI, sepsis and C. difficile. The challenge for ID physicians is convincing hospital and health system leaders that ID attribution to these measures is real and that improvement in these measures adds value to the institution. From there, innovating reimbursement and compensation models can be explored.
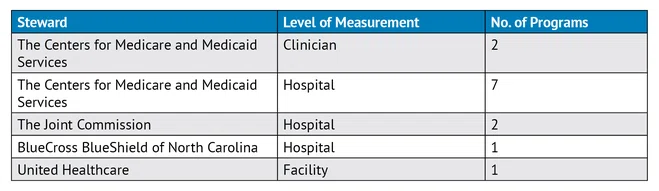
TABLE 1: Quality Reporting Programs Relevant to ID