Previous Page
${prev-page}
Next Page
${next-page}




Market and Practice Landscape
For all physicians, including ID physicians, to thrive in a value-based contract or quality-based compensation incentive, it is important to consider the market in which they operate and services they provide.
A. Market Considerations
These considerations include the size of the market in which a physician operates (i.e., number of beds covered and total population within the service area), local geography and competition (i.e., large metropolitan area with many ID physicians/practices versus small rural community with few ID physicians/practices).
B. Practice Considerations
These considerations include the services being offered by an ID physician or practice. The list of potential services is long and variable depending on the market considerations but can range from comprehensive ID services (e.g., a physician or practice being responsible for all ID-related activities, clinical and administrative) to a single ID service (e.g., infection control, antimicrobial stewardship, COVID‑19/special pathogens medical director).
C. Spectrum of Measures of Quality to Value
After considering the market and practice dynamics for an ID physician or practice, the selection of the appropriate quality- or value-based metric becomes simpler yet still imperfect until ID-tailored metrics are developed.
The level of adoption for ID will vary by practice location and organizational progress in codifying metrics and goals across the spectrum of advancement within quality and value domains. Figure 2 provides a summary of this quality-to-value spectrum. On the left are quality measures that are considered introductory, and on the right are more complex population health measures. The adoption of quality- or value-based metrics is generally dependent on the convergence of organizational and/or payer appetite for contributing funding to a compensation or reimbursement program. Hospitals, health systems and academic medical centers often already have significant dollars at risk for performance in metrics in which ID physician activities are attributable.
As shown in figure 2, the spectrum of measures from quality to value generally follows a less-complex-to-more-complex progression based on the ability to measure the metric, attribute the improvement of the metric and create clear and defined baseline expectations. Importantly, it is a spectrum, and different organizations may be at different points in their respective progress toward value-based care and the development of metrics measured within the organization (moving from the left side of the table to the right side). Most metrics in figure 2 are appropriate for all ID settings (private practice, AMC and health system), but organizations tend to select only a few metrics to measure and track for a specialty. That said, employer type can be an initial indicator for where an organization might be in that evolution.
• Single-physician practices and private practice physicians tend to gravitate toward quality metrics on the left side of figure 2. The implementation of these metrics can be highly controlled and maintained in a smaller scope of practice with limited (if any) inpatient responsibilities. These metrics also typically have existed for long enough to ensure clear operational baseline expectations exist at the provider level.
• AMCs and physicians employed by AMCs tend to progress toward metrics with a moderate level of complexity and adoption (middle of the spectrum).
• Lastly, large integrated health systems have advanced the furthest, toward the most complex metrics that can be implemented at a large scale (toward the right side of the spectrum).
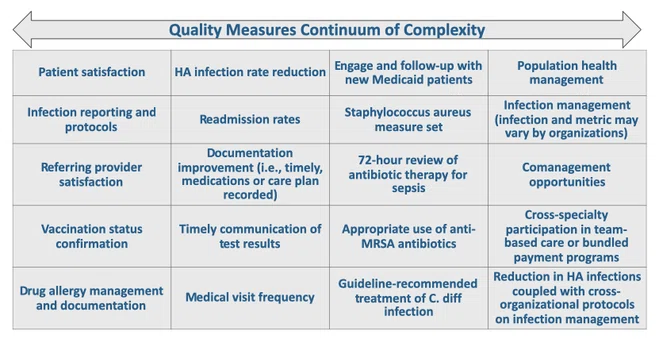
FIGURE 2: Spectrum of Measures, From Quality to Value